Welcome to
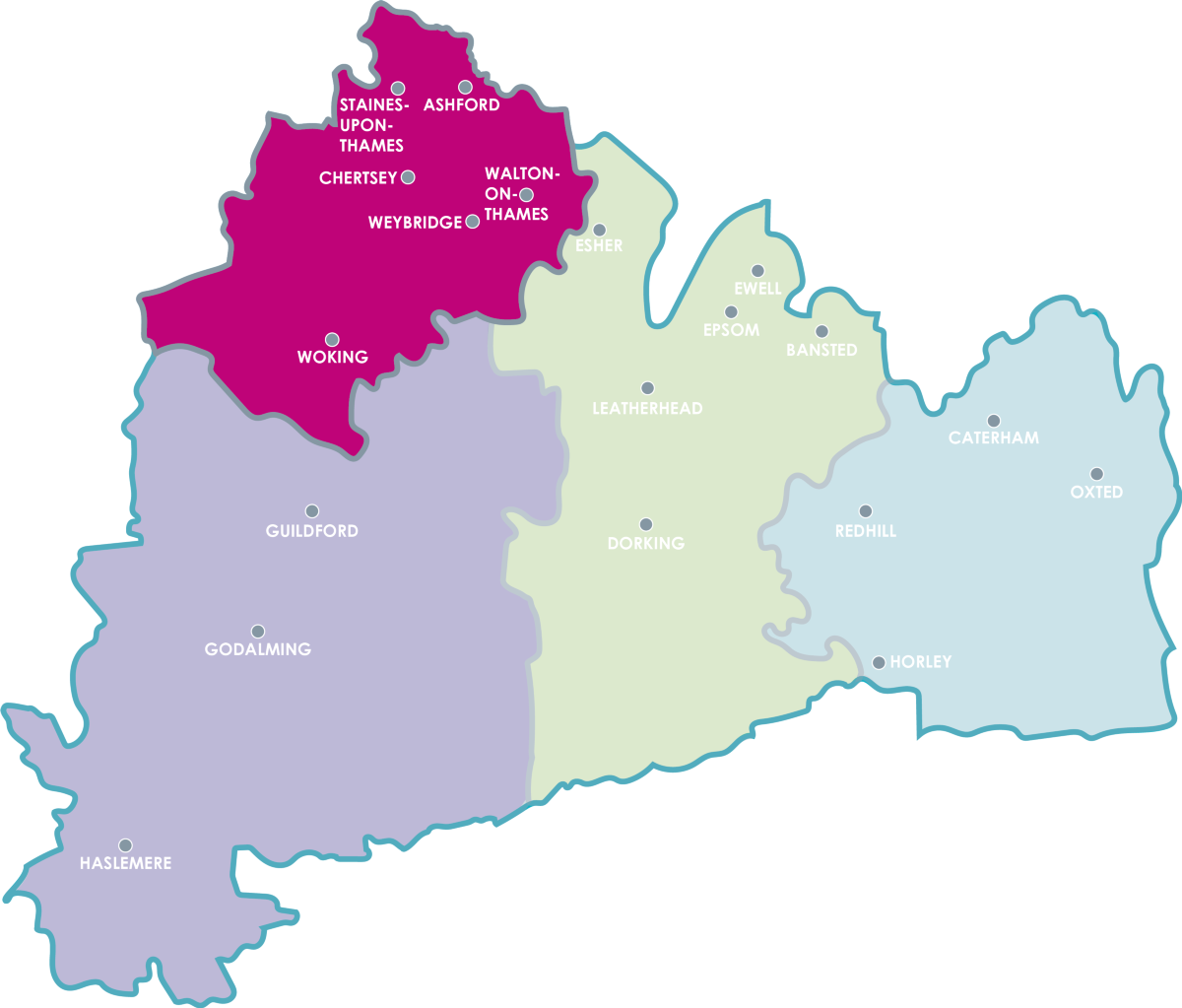
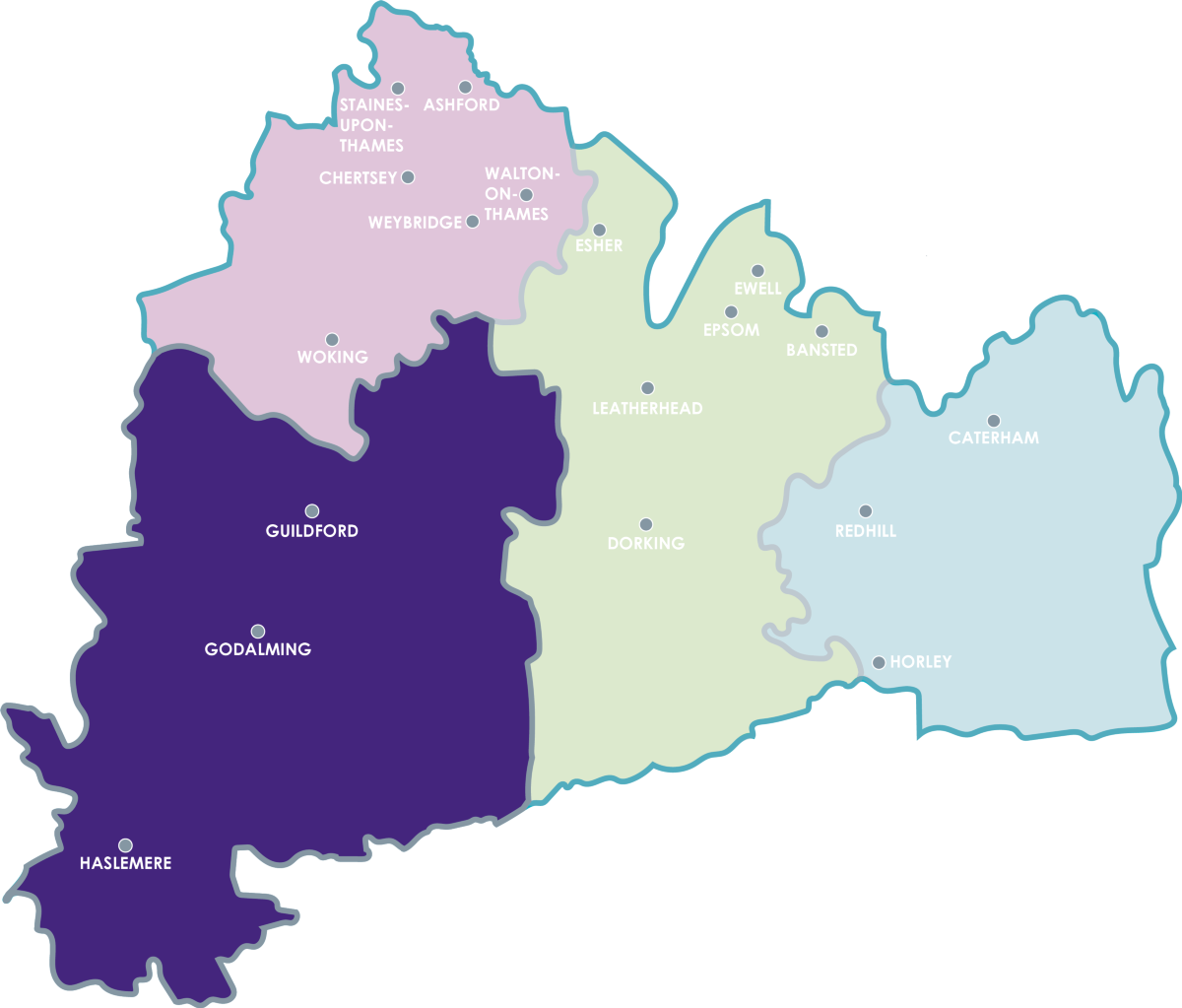
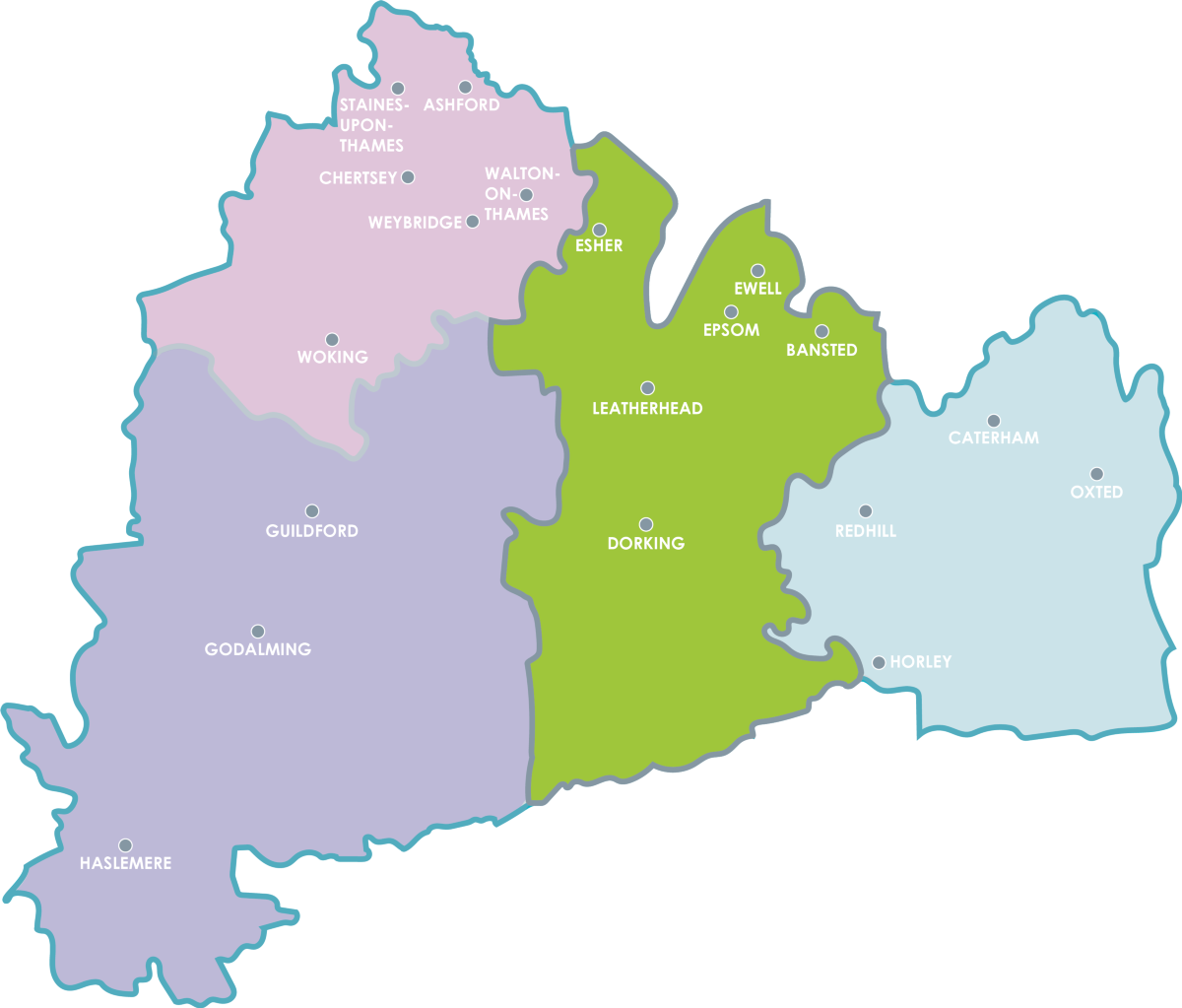
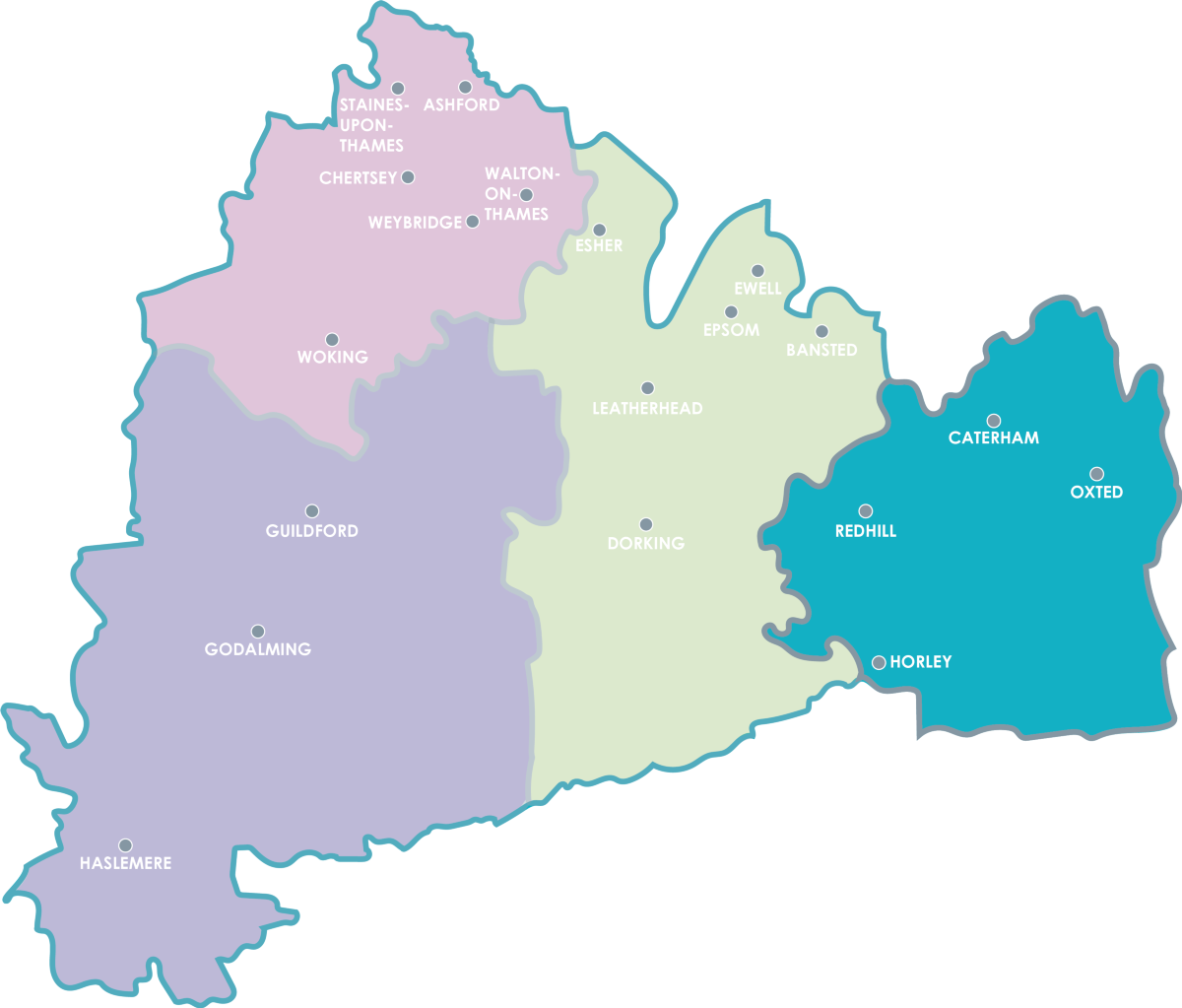
Surrey Heartlands Health and Care Partnership

- Surrey Heartlands is a partnership of organisations working together – with staff, patients, their carers, families and the public – to support people to live healthier lives.
What are you looking for?
We can help you access information, answer your questions and concerns or point you in the right direction.
Want to find out more about us and what we do? We have you covered.
Top enquiries
Covid-19 vaccination programmeFlu vaccination programmeAccess a serviceHow do I register with a GP practice?Pharmacies and prescriptionsHow do I make a complaint?I'm looking for a career in Health and Social careCurrent vacancies in Surrey HeartlandsFind out about Continuing HealthcareMake an Individual Funding RequestApply for a Personal Health BudgetI have a Freedom of Information request
Joining up care across Surrey Heartlands
Having a clear strategy in place is vital and allows us to focus on how best to meet the health and wellbeing needs of people in Surrey and reduce the inequalities we know currently exist.
As a health and care partnership we want to work with our communities to harness local innovation, so residents can access the right support that’s developed from the ground-up, with joined up health and care services that make the most of digital technology.
Read our strategy and watch this video to find out more.
News centre

The Prime Minister, Rishi Sunak visited the Woking Community Hospital on Thursday 11 April 2024 with Woking MP, Jonathan Lord, to meet with staff and learn more about the Community Diagnostic Centre (...

A discharge programme, which has helped more patients return home sooner after receiving care in East Surrey, was a finalist in the prestigious Health Service Journal (HSJ) Partnership Awards. Deve...

Surrey Heartlands’ Joint Chief Medical Officer urges people to ‘Help us, help you’ ahead of the Easter bank holiday weekend As the NHS prepares for what’s expected to be ano...
News and stories from around Surrey Heartlands, from and for the people it serves. View it all via our news centre, including videos and case studies.
Choose the right NHS service
Introducing the Heart Beetz, a band who have been recording their latest hit while battling with illness and minor accidents. Inspired by their own experiences of NHS services they’ve released a track about getting help from the right place if you’re unwell or injured.

Working collaboratively to improve long-term health and care in Surrey Heartlands
We all want people in Surrey to live in good health for as long as possible and that they are supported to get the right help, when and where they need it.
Read about how we plan to do this over the coming years, working in partnership with both our workforce and local people, and continue to support the people of Surrey Heartlands to live healthier lives.
Looking ahead: Our vision for health and care in Surrey Heartlands

Our commitment to equality, diversity and inclusion
Equality, diversity and inclusion is at the core of our values at Surrey Heartlands and we will continue to take a dynamic and collaborative approach to celebrate and embrace diversity.